Update 9/30/2015: We're in the home stretch. If you need last-minute in-depth information about the ICD/DSM transition, register to view our webinar or contact eHana directly.
October 1st, 2015 is arriving quickly. That's the date when the Center for Medicare & Medicaid Services (CMS) has mandated that healthcare providers and payers switch over to the new ICD-10 coding system. In addition, behavioral health providers will generally be required to switch to DSM-5, the newer version of the DSM-IV-TR diagnosing standard that has been in use for over a decade and a half.
This presents a number of organizational and technical challenges for provider agencies. (In addition to this blog post, our team conducted an informative ICD-10 & DSM-5 webinar you can register to view.)
ICD-10
To begin with -- what is the ICD-10, and how does it differ from the ICD-9 codes we're currently using?
Summary of changes for ICD-10
ICD-10 was introduce to improve the accuracy of billing and reporting, as well as to provide better international public health reporting. ICD-10 expands upon the ICD-9 code set significantly. It also heavily revises the previous ICD code format (XXX.XX) with a new, three to seven-character coding system in the following format:
Because of the dramatically expanded number of codes, there are some hilarious examples of codes. The example above is the code for "Struck by Orca", which is available in a humorous book of the same name from ICD10Illustrated.com.
The good news, as it pertains to behavioral health providers at least, is that the "F" codes used by providers, tends to be much simpler than the broader set of ICD-10 codes.
"F" Codes for Mental, Behavioral. and Neurodevelopmental disorders
DSM-5
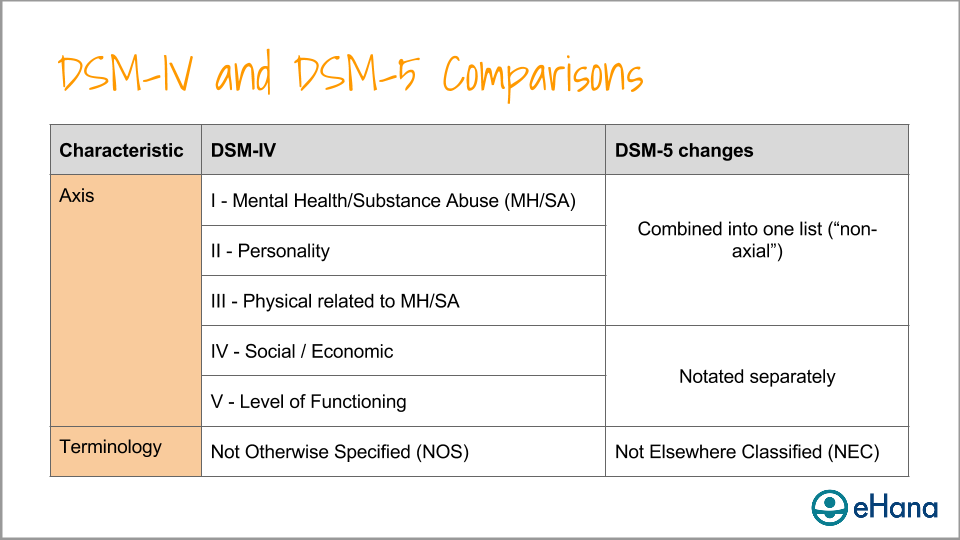
The DSM-5 also represents a substantial change, both on a structural level (no more "Axes") and from a content perspective.
Comparison between DSM-IV and DSM-5
Among other changes, in the DSM-5, disorders have been added, category names revised or eliminated, disorders have been re-categorized, the criteria has been changed for many existing disorders, and specifiers and severity indicators have been added.
"Mapping"
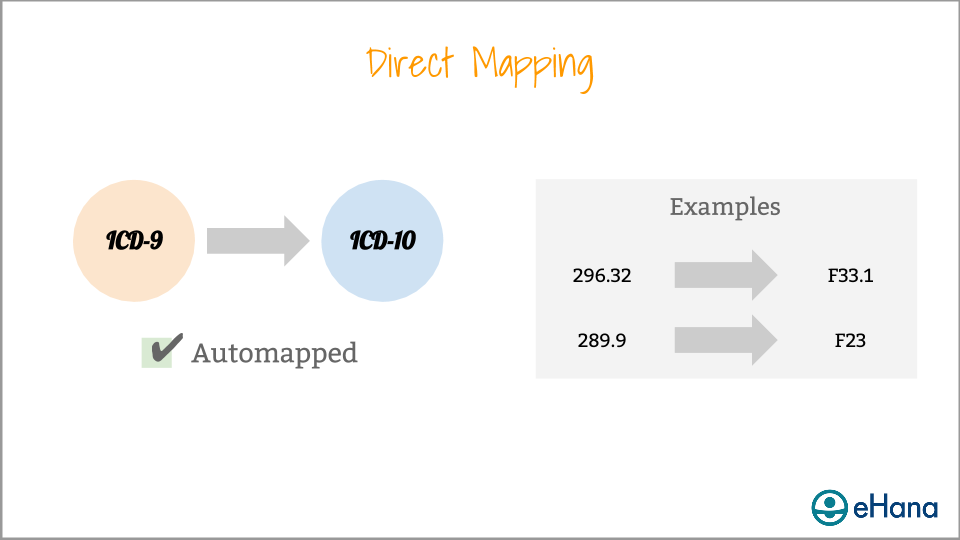
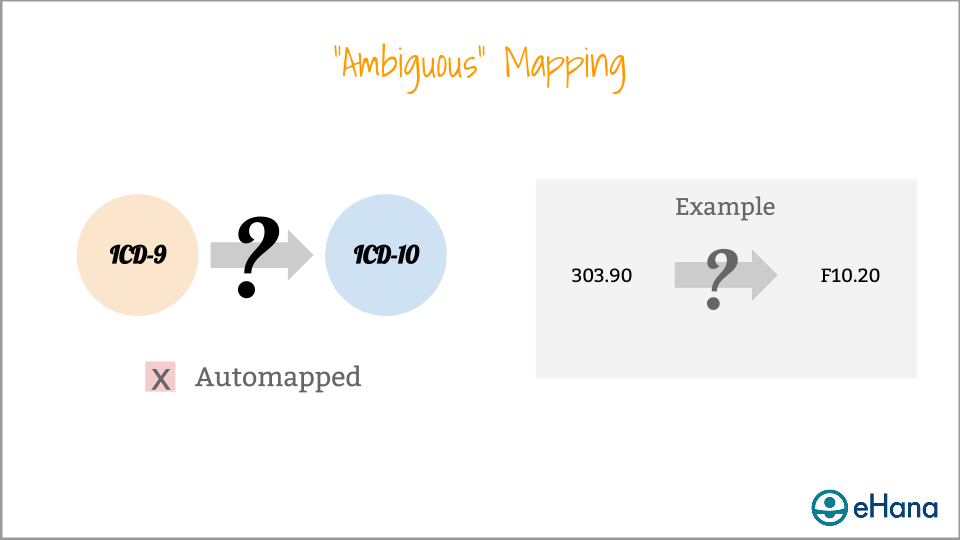
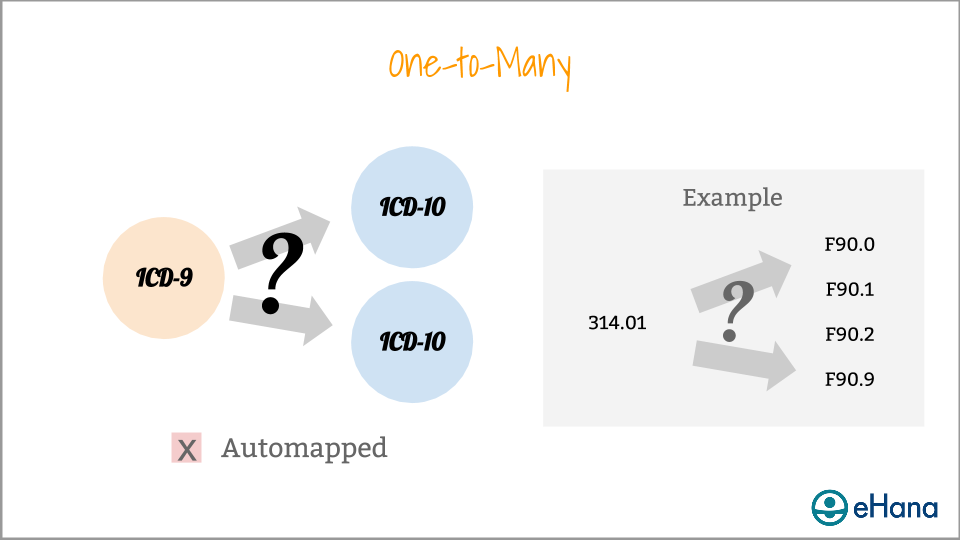
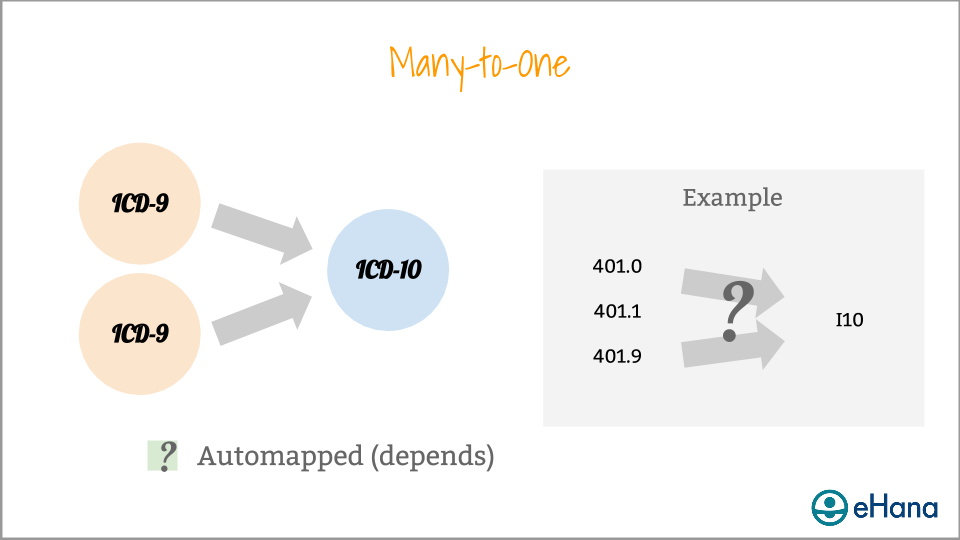
One of the biggest transition questions agencies face is how to map from the ICD-9 to the ICD-10. There are many different types of mappings.
The type of mapping available for a given code determines the ease at which a diagnosis can be translated from ICD-9 to ICD-10. In our (eHana's) experience, the typical behavioral health provider can expect to automatically map about 50% of its active billing diagnoses.
Managing the transition
The impact of the ICD-10 and DSM-5 transition is widespread, with effects throughout a typical provider organization. Billing is at risk based on staff, EHR, billing system, or payer readiness; operational processes will be reassessed around new code categories; and documentation and delivery of clinical care, as well as quality assurance, are impacted.
Broadly speaking, eHana's recommended transition plan involves:
Gathering information and assessing impact
Developing a transition plan
Engaging and training clinical staff
Developing a back-up plan
Auditing and monitoring clinical and billing records
For more detailed planning information, watch eHana's ICD-10 & DSM-5 Transition Webinar.
eHana Readiness
eHana EHR is 100% ready to support your agency's transition to ICD-10 and DSM-5. Because of our web-based "Software as a Service" approach, the new codes were rolled out, and the existing clients automatically mapped where possible, without any workflow interruption or new software to install.
Confused? Need more information?
We're here to help. The eHana team has over 15 years of experience in helping agencies manage regulatory changes. Earlier this year, we conducted a webinar covering the ICD-10 and DSM-5 transition, which we encourage you to view.